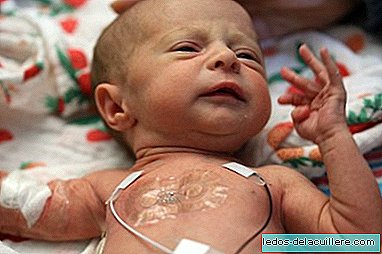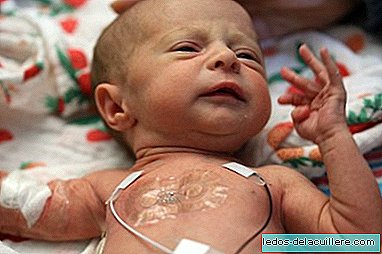
He is born and his body is smaller than normal, because he was born too early. He needs the heat of the body of mom and dad, but it is not possible, because he needs to be hooked on a multitude of wires that control his breathing and his heart rate is adequate, since his organs are not yet mature enough.
It is the reality of a premature. You can't help having him in this cold environment, so far, at least! A group of 45 pediatricians, dermatologists and engineers from Northwestern University in Illinois (USA) has developed a wireless biosensor located under the crib mattress, which records the vital signs of newborns and can be controlled from an app, accessible from a smartphone or tablet.
In this way, medical staff can monitor the baby at all times but allowing parents to cuddle and make skin with skin without wires in between, the best medicine for the baby.
Proven: measure more than the traditional monitor

As explained by the interdisciplinary team at Northwestern University in Chicago, they have created soft and flexible sensors, the first to monitor babies in the Neonatal Intensive Care Unit (NICU) with precision and without wires.
These medical personnel have completed the first studies in premature babies, at the Prentice Women's Hospital and at the Ann & Robert H. Lurie Children's Hospital in Chicago, and have verified that the wireless sensors provided data as accurate and accurate as those of the traditional monitoring systems.
The wireless patches are also softer on the fragile skin of the newborn and allow greater skin-to-skin contact with parents.
The study, published in the journal Science, includes initial data from more than 20 babies who used wireless sensors along with traditional monitoring systems, so researchers could compare between them. Since the end of the study, the team has proven its effectiveness in more than 70 babies in the NICU.
 In Babies and more Born prematurely, an arrival in the world ahead of time for which no one is prepared
In Babies and more Born prematurely, an arrival in the world ahead of time for which no one is preparedJohn A. Rogers, a pioneer of bioelectronics, who co-led the development of these sensors with dermatologists Amy Paller and Shuai (Steve) Xu, explains:
"We wanted to eliminate the mess of aggressive cables and adhesives associated with existing monitoring systems and replace them with something safer, more patient-centered and more compatible with parent-child interaction."
And it seems that they have succeeded:
"Our wireless, battery-free and skin-like devices are equally accurate in measurement, and even provide advanced measurements that are clinically important but are not often collected among premature babies.
In fact, Traditional monitors measure:
Heart rate
Breathing frequency
Body temperature
Blood oxygen levels
Roger's new wireless sensor from the team monitors, in addition to the previous four:
Blood pressure
Blood flow
Vital functions during parent-child interactions
The best benefit: skin to skin with mom and dad
Just as important as monitoring the baby, according to Paller, a pediatric dermatologist, is to encourage contact with his parents.
"It has been shown to decrease the risk of lung complications, liver problems and infections. However, it is very difficult for a mother to hug her baby, if there are wires everywhere and the newborn is tied to a bed."
And he says it with knowledge of the cause, since the mass of ables surrounding newborns in the NICU is usually larger than the size of the baby itself.
Traditionally five or six wires connect each baby's electrodes to breathing monitors, blood pressure, blood oxygen, heartbeats ...
Although these cables guarantee health and safety, they limit the baby's movements and constitute an important barrier to the physical bond during a critical period of development.
 In Babies and more, stroking, hugging and talking to premature babies is key to improving their development
In Babies and more, stroking, hugging and talking to premature babies is key to improving their developmentHow do the new wireless sensors work?
 Dual chest sensor and single foot sensor, provided by Northwestern University.
Dual chest sensor and single foot sensor, provided by Northwestern University. - Dual wireless sensors control the vital signs of babies (heart rate, respiratory rate and body temperature) from opposite ends of the body. One sensor (measuring five centimeters by 2.5 centimeters) is located on the baby's chest or back, while the other sensor (2.5 centimeters by 2 centimeters) is wrapped around one foot.
This strategy, as the team manager explains, It allows to obtain the central temperature and body temperature of a baby from a peripheral region.
"The temperature differences between the foot and the chest are of great clinical importance in determining blood flow and cardiac function, something that is not normally done today."
Doctors can measure blood pressure continuously tracking the heart pulse to the foot. Currently, there is no good way to obtain a reliable measurement of blood pressure. A bracelet to measure blood pressure can cause bruising or damage the baby's fragile skin. The other option is to insert a catheter into an artery, which is delicate due to the small diameter of the blood vessels of a premature newborn.
It could also help fill in the information gaps that exist during skin-to-skin contact. By being able to measure the vital signs of babies while they are in the arms of their parents, you can learn more about the importance of this contact.
Being transparent, the sensors can be used during x-rays, magnetic resonances and tomographs.
It could be available in two years
That is what is assured in the journal Science: that in two or three years it could be used in a normalized way in the United States, although work is being done to reach other countries with less economic resources such as Zambia or India or Pakistan.
Another advantage commented by its inventors is its low cost: Each patch costs about 9 euros, and since more than one device (up to six) can be connected remotely to a single mobile or tablet, devices could be saved. A single nurse or a doctor can monitor several babies.
If you still have doubts about the operation of these sensors, I encourage you to see this video prepared by the university itself where the invention was made.
Via and photos | Northwestern University